A research group from Duke led by CVIT and CIPG researchers, recently published an article about a new holistic model to assess total risk in radiology. This study also involved researchers from the Department of Biostatistics & Bioinformatics and defined a new approach where radiation risk is put in perspective with imaging benefits.
Balancing risk and benefit is essential for safe and effective radiology practices. However, this comparison can be hard because risks and benefits are measured in different ways. While many strategies have been developed to ascertain radiation risk, there has been a paucity of studies assessing clinical risk, thus limiting the ability to minimize overall risk to patients undergoing imaging examinations.
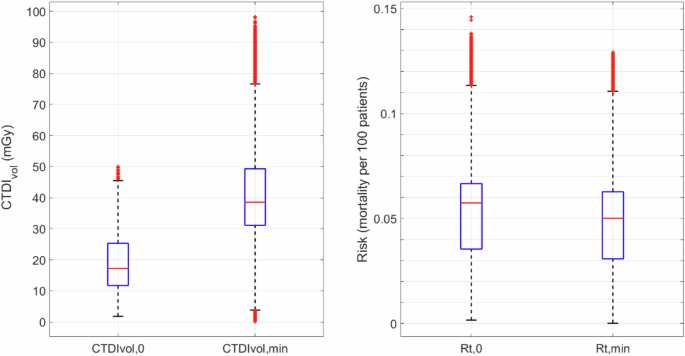
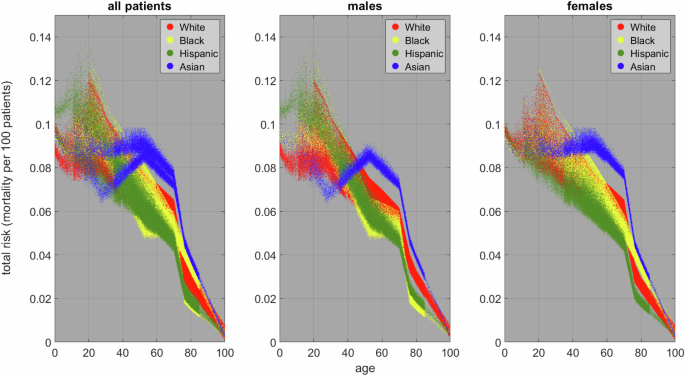
To address this, Duke researchers proposed a model to characterize total risk that combines radiation and clinical risks. These risks are calculated as functions of multiple factors, including radiation dose, disease prevalence, false-positive rates, expected life-expectancy loss due to misdiagnosis, and radiologist interpretative performance (i.e., AUC).
The model was applied to a simulated population of one million cases in a liver cancer scenario. Results revealed that, for all demographics, clinical risk outweighed radiation risk by at least 400%. This finding underscores the importance of not overly focusing on dose reduction, as excessively low doses can compromise diagnostic accuracy and patient care. Moreover, the study found that optimizing typical abdominal CT exams should involve a radiation dose increase in over 90% of the cases. These results highlighted the dominance of clinical risk at typical CT examination dose levels, and exaggerated dose reductions can even harm patients.
This pioneering work provides a vital framework for optimizing radiology practices by focusing on minimizing total risk. It has the potential to transform imaging protocols, ensuring safer and more effective diagnostic outcomes for patients.